 web3.0
web3.0
 Ped-BERT: Early Detection of Diseases and Length of Hospital Stay Prediction for Pediatric Patients
Ped-BERT: Early Detection of Diseases and Length of Hospital Stay Prediction for Pediatric Patients
Ped-BERT: Early Detection of Diseases and Length of Hospital Stay Prediction for Pediatric Patients
Early identification of diseases and their associated length of hospital stay (LoS) is vital for better treatment options, more effective follow-up arrangements, longer survival rates, improved long-term outcomes, and lower hospital utilization costs.
Early identification of diseases and their associated length of hospital stay (LoS) is vital for better treatment options, more effective follow-up arrangements, longer survival rates, improved long-term outcomes, and lower hospital utilization costs.
In recent years, breakthrough progress in diagnosis prediction was made by leveraging electronic health records (EHR) and advanced deep learning (DL) architectures, such as convolutional neural networks (CNN, e.g., Nguyen et al. (Deepr)1), recurrent neural networks (RNN, e.g., Choi et al. (Doctor AI)2), long short-term memory networks (LSTM, e.g., Pham et al. (DeepCare)3), and an even more powerful architecture called Bidirectional Encoder Representation from Transformers (BERT). For instance, Li et al.4 introduce BEHRT, a BERT-inspired model applied to EHR, capable of predicting the likelihood of more than 300 conditions in one’s future medical visit; Shang et al.5 propose G-BERT, a model that combines the power of graph neural networks (GNN) and BERT for diagnosis prediction and medication recommendation; Rasmy et al.6 introduce Med-BERT, also a BERT model, to provide pre-trained contextualized embeddings run on large-scale structured EHR. However, a very limited number of studies focus on leveraging EHR and state-of-the-art DL architectures for the task of predicting hospital LoS7,8. For instance, Song et al.7 develop SAnD (Simply Attend and Diagnose), a DL-inspired model, to predict diagnosis codes and LoS, among other tasks, using a multi-class classification approach. Their LoS estimation is based on analyzing events occurring hourly from admission time. Additionally, Hansen et al.8 introduce M-BERT, a BERT-inspired model applied to sequences of patient events gathered within the first 24 h of admission for binary, multi-class, and continuous LoS prediction.
To the best of our knowledge, most advances in this literature (a) rely on EHR representative of the adult population4,7,9; (b) need to specify the patient age distribution1,2,5,6,8,10,11,12,13; (c) estimate how long a patient is likely to stay in the hospital after being admitted, however, forecasting LoS before admission is equally pertinent in preventive healthcare and optimizing hospital resource allocation7,8; (d) use models that focus on predicting diagnosis or LoS for a limited set of health outcomes3,10,14; (e) focus on improving health risk assessment performance by accounting only for the timing irregularity between clinical events (e.g., age at the time of visit)1,2,4,8; (f) do not report prediction performance on rare diseases15, or (g) do not use in-utero health information for diagnosis prediction.
However, computer-aided early detection of diseases and their associated LoS holds particular significance in the field of pediatrics. Timely diagnosis and intervention are crucial for enhancing the long-term well-being of children, as highlighted in various studies14,15,16,17,18. Consequently, we develop Ped-BERT, an architecture inspired by BERT19. Our model accurately predicts over 100 potential primary diagnoses and the length of hospital stay that a child might face during their upcoming medical visit, by relying on pre-trained diagnosis embeddings. We evaluate our approach against two contemporary classifiers (a logistic regression and a random forest) and two state-of-the-art DL classifiers (a pre-trained transformer decoder and a neural network with randomly initialized embeddings). Thus, our analysis could serve as a valuable tool for assisting researchers in utilizing machine learning for pediatric healthcare guidance, therefore aiding pediatricians in their clinical decision-making processes.
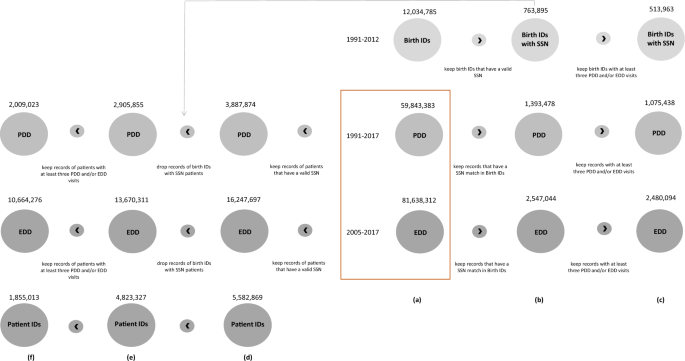
Ped-BERT leverages a rich dataset encompassing hospital discharge records and emergency room information for pediatrics, including the patient’s age and the residential zip code or county at the time of the visit. Additionally, it can optionally integrate maternal health data from both pre- and postnatal periods. To the best of our knowledge, our prediction framework, leveraging data that matches mother and baby pairs longitudinally is the first of its kind. Furthermore, this dataset empowers us to explore the model’s capability to simultaneously predict primary diagnosis and LoS in the next medical visit, and to assess its overall fairness, including an examination of whether prediction errors are evenly distributed across different demographics of mother–baby pairs.
In summary, we contribute to the literature as follows: first, we use a novel data set that links medical records of mother–baby pairs between 1991 and 2017 in California; second, we develop Ped-BERT, a DL architecture for early detection prediction of health risks for pediatric patients seeking care in inpatient or emergency settings, and compare its performance against other contemporary or state-of-the-
The above is the detailed content of Ped-BERT: Early Detection of Diseases and Length of Hospital Stay Prediction for Pediatric Patients. For more information, please follow other related articles on the PHP Chinese website!

Hot AI Tools

Undresser.AI Undress
AI-powered app for creating realistic nude photos

AI Clothes Remover
Online AI tool for removing clothes from photos.

Undress AI Tool
Undress images for free

Clothoff.io
AI clothes remover

Video Face Swap
Swap faces in any video effortlessly with our completely free AI face swap tool!

Hot Article

Hot Tools

Notepad++7.3.1
Easy-to-use and free code editor

SublimeText3 Chinese version
Chinese version, very easy to use

Zend Studio 13.0.1
Powerful PHP integrated development environment

Dreamweaver CS6
Visual web development tools

SublimeText3 Mac version
God-level code editing software (SublimeText3)

Hot Topics
 1663
1663
 14
14
 1420
1420
 52
52
 1313
1313
 25
25
 1266
1266
 29
29
 1239
1239
 24
24
 Nasdaq Files to List VanEck Avalanche (AVAX) Trust ETF
Apr 11, 2025 am 11:04 AM
Nasdaq Files to List VanEck Avalanche (AVAX) Trust ETF
Apr 11, 2025 am 11:04 AM
This new financial instrument would track the token's market price, with a third-party custodian holding the underlying AVAX
 OM Mantra Cryptocurrency Crashes 90%, Team Allegedly Dumps 90% of Token Supply
Apr 14, 2025 am 11:26 AM
OM Mantra Cryptocurrency Crashes 90%, Team Allegedly Dumps 90% of Token Supply
Apr 14, 2025 am 11:26 AM
In a devastating blow to investors, the OM Mantra cryptocurrency has collapsed by approximately 90% in the past 24 hours, with the price plummeting to $0.58.
 Zcash (ZEC) Reaches a High of $35.69 as a Record Amount of Tokens Move Out of Circulation
Apr 09, 2025 am 10:36 AM
Zcash (ZEC) Reaches a High of $35.69 as a Record Amount of Tokens Move Out of Circulation
Apr 09, 2025 am 10:36 AM
Zcash was one of the top gainers during the latest market rally, reaching a high of $35.69 as traders moved a record amount of tokens out of circulation.
 Is Wall Street Quietly Backing Solana? $42 Million Bet Says Yes
Apr 10, 2025 pm 12:43 PM
Is Wall Street Quietly Backing Solana? $42 Million Bet Says Yes
Apr 10, 2025 pm 12:43 PM
A group of former Kraken executives acquired U.S.-listed company Janover, which secured $42 million in venture capital funding to begin building a Solana (SOL) treasury.
 TrollerCat ($TCAT) Stands Out as a Dominant Force in the Meme Coin Market
Apr 14, 2025 am 10:24 AM
TrollerCat ($TCAT) Stands Out as a Dominant Force in the Meme Coin Market
Apr 14, 2025 am 10:24 AM
Have you noticed the meteoric rise of meme coins in the cryptocurrency world? What started as an online joke has quickly evolved into a lucrative investment opportunity
 Dogecoin (DOGE) Price Plummets 17%
Apr 08, 2025 am 11:20 AM
Dogecoin (DOGE) Price Plummets 17%
Apr 08, 2025 am 11:20 AM
The Dogecoin price plummeted 17% in the last 24 hours to trade at $0.1365 as of 4.30 a.m. EST on trading volume that skyrocketed 271% to $2.24 billion.
 As Fear Drives Selling, BlockDAG (BDAG) Stands Out from the Crowd
Apr 13, 2025 am 11:48 AM
As Fear Drives Selling, BlockDAG (BDAG) Stands Out from the Crowd
Apr 13, 2025 am 11:48 AM
As fear drives selling in the crypto market, major coins like Cardano and Solana face tough times.
 The Crypto Market Has Witnessed a Rebound Following the Recent Sheer Downturn
Apr 13, 2025 am 11:40 AM
The Crypto Market Has Witnessed a Rebound Following the Recent Sheer Downturn
Apr 13, 2025 am 11:40 AM
The crypto market has witnessed a rebound following the recent sheer downturn. As per the exclusive market data, the total crypto market capitalization has reached $2.71Ts


