 Technology peripherals
Technology peripherals
 AI
AI
 Barriers to widespread adoption of artificial intelligence in healthcare
Barriers to widespread adoption of artificial intelligence in healthcare
Barriers to widespread adoption of artificial intelligence in healthcare
Artificial Intelligence (AI) has the potential to significantly improve healthcare delivery. As AI is able to unlock insights and patterns from very large data sets, it lays the foundation for innovative, high-value, enhanced capabilities such as prediction of patient deterioration, recommendations for appropriate intervention for specific conditions, and high-frequency monitoring of many vital signs in parallel. Analysis and Insights. CalmWave founder and CEO Ophir Ronen discusses the barriers to AI adoption and how the healthcare industry can overcome them.

However, the healthcare industry is particularly cautious in adopting artificial intelligence, according to a recent Brookings Institution report opens a new window. While it's natural to treat new technologies with caution, this is especially true in the healthcare world, where providing the best care for patients involves tremendous responsibility. There are many factors that clinicians worry about when adopting artificial intelligence, including fear of being marginalized, fear that errors caused by AI will have a negative impact on patient health (i.e., death), and fear that conclusions based on black-box AI are not well understood.
Before exploring these questions, it is important to understand what healthcare providers will gain from artificial intelligence, especially when it comes to working conditions.
What can artificial intelligence do for health care?
Artificial intelligence has the potential to revolutionize health care by enhancing clinicians’ ability to identify and treat disease. AI systems can analyze large amounts of data from electronic health records, imaging studies and other sources to find patterns that would be difficult for humans to spot. These analyzes can lead to earlier, more accurate diagnoses, better treatment outcomes and more personalized care.
One area where artificial intelligence can have a significant impact is in reducing clinician burnout. Nurses, in particular, are at risk of burnout due to the high demands of their jobs. Artificial intelligence can help alleviate this problem by providing an objective measure of workload based on the frequency of ICU alerts, patient acuity, and the frequency and complexity of interventions. Enabling hospital administrators and managers to understand clinician workload and likelihood of burnout can promote data-driven opportunities to make the workplace healthier, where clinicians want to stay and follow their passion for treatment.
In addition to reducing burnout, AI can help clinicians make more informed decisions by integrating real-time data to provide actionable insights and predictive analytics. For example, AI algorithms can analyze patient data to identify patients at risk for complications and alert clinicians to take preventive measures. This can improve patient outcomes and reduce healthcare costs by avoiding more serious complications.
Overall, artificial intelligence has the potential to transform health care by enhancing clinicians’ ability to analyze large amounts of data and identify patterns that are difficult for humans to detect. By reducing burnout, providing real-time data and predictive analytics, AI can help clinicians make more informed decisions, improve patient outcomes, and reduce healthcare costs.
Common Barriers to Widespread Adoption of Artificial Intelligence
Artificial intelligence seems to be the key to making the lives of health care workers easier. However, there are several risks in introducing complex and unfamiliar technology into such an important industry. In fact, many health care workers worry that AI will do more harm than good to providers and patients.
Here are a few reasons why healthcare providers may be resistant to AI:
1. Explainability
Perhaps the biggest obstacle to the adoption of AI in healthcare is Mysteries surrounding the mechanics of artificial intelligence. How do these algorithms work? How are the above data points generated? “Black box” AI is a thing of the past, and clinicians (and regulators) expect explanations when it comes to AI-based solutions.
"Explainability" refers to the concept that a machine learning model and its output can be explained in a "meaningful" way at a human-acceptable level. In order to confidently implement artificial intelligence into their operations, healthcare practitioners must demonstrate that it will abide by the Hippocratic Oath, which is to "do no harm." Without a thorough understanding of how AI makes decisions, it will be difficult for practitioners to hand over important responsibilities to machines.
2. Bias and Discrimination
Many health care systems are steadily increasing their efforts to address racial disparities and expand access to services for minority and underserved communities. Unfortunately, medicine has a long history of bias. In some cases, artificial intelligence is used to exacerbate the problem.
Practitioners may worry that AI algorithms trained on specific data sets will systematically ignore companywide initiatives to improve health equity, thereby perpetuating discriminatory practices. Any AI-based technology in healthcare today must consider these dynamics when developing more comprehensive and powerful solutions to improve care for everyone.
3.Risk and Comfort
Technology will never be perfect. Healthcare providers strive for perfection because anything less than perfect can mean lives are compromised. The stakes in health care are high, and so are the expectations for any new medical technology. AI-based products are very accurate, but not perfect. Therefore, new technologies based on artificial intelligence may still lead to some errors or failures that may lead to misdiagnosis or mistreatment of critically ill patients. This expectation is not unique to AI, but it does create a high and sometimes unrealistic bar that slows adoption. Additionally, legacy systems face ongoing challenges.
Different organizations have their own systems and methods of patient care. Suppliers often view familiarity and consistency as more important than sophistication and accuracy. A technology is not necessarily good or accurate enough, but it is equally important to consider the clinician's comfort level using and understanding the technology.
4. Lack of Regulation
Although the FDA has approved hundreds of artificial intelligence medical devices, there are no relevant regulations for non-commercial artificial intelligence algorithms in healthcare. The challenge in crafting these regulations stems largely from the speed at which artificial intelligence is developing. This seeming lack of oversight and accountability is understandable for healthcare workers, who would prefer to know that the new technology has been approved by regulators and adhered to certain standards, particularly around privacy and anonymity. aspect.
How to Introduce Artificial Intelligence into Healthcare
Despite the reservations of clinicians, artificial intelligence can and will change the face of healthcare. However, to successfully implement AI-based tools, clinicians must be at the forefront of designing, testing, and training new medical technologies.
Design
To give trust to an AI system, healthcare practitioners must be directly involved in its design and implementation. You can’t blame clinicians, who expect AI developers to share their goals and be fully aware of their concerns.
Hospitals are complex ecosystems with critical workflows. Successfully integrating AI into healthcare systems requires a comprehensive look at existing workflows to improve them rather than add more work. Including health workers in the design phase is critical to ensuring that AI prioritizes usability and integrates seamlessly into daily workflows.
Transparency
Developers of AI systems must provide practitioners with full visibility and transparency into the AI decision-making process. Provide users with not only the end result of the process, but also data to support decision-making. Without this basic requirement, the future of AI in critical care functions seems remote. Clinicians must feel they agree with the design of the algorithm and the data processed by the AI to deliver the desired results.
User Testing
To this end, healthcare workers should have adequate opportunities to test artificial intelligence in clinical settings. These real-world interactions will ultimately reveal which use cases support care delivery for practitioners and patients, and which use cases create unnecessary complications.
Simply rolling AI technology into hospital wards without providing user testing to clinicians will exacerbate clinician concerns about unfamiliarity, bias and risk of failure. Getting clinicians accustomed to using the technology from the outset will alleviate their concerns and improve integration. Additionally, feedback from healthcare professionals will ultimately help AI companies continually improve their technological capabilities to streamline daily tasks and address practitioners’ most pressing needs.
Clinical Evidence
There is one thing that guarantees approval from a healthcare provider: certification. Much healthcare follows a clinical evidence-based approach. Clinical evidence-based medicine (EBM) is a medical practice approach that emphasizes the use of the best available research evidence to guide clinical decisions. The goal of EBM is to improve the quality of patient care by ensuring that treatments and interventions are based on the latest and most reliable scientific evidence. The key word here is evidence.
While this takes more time and may seem like a huge inconvenience and adoption barrier, it is often a necessary step to ensure a safe and sustainable solution. To be clear, there are varying degrees of evidence and the healthcare industry (including regulators) must adapt to conditions, scenarios and exceptions to provide appropriate flexibility to accelerate the use of the technology. Putting evidence behind technology not only improves patient care but also instills the confidence clinicians need to drive adoption.
Health care providers: The purpose of artificial intelligence is to enhance your capabilities
The healthcare industry’s reservations about artificial intelligence are undoubtedly reasonable and deserve to be taken seriously. Start by acknowledging the changes that AI will bring and dispelling the notion that the introduction of AI will immediately modernize the industry.
It is important for healthcare professionals to know that without their input, AI will not be adopted and any AI initiative will have clearly defined goals, values and evidence. Clinicians can, should, and must have a say in the design, testing, and implementation of AI technologies. There is no health care without clinicians. As more healthcare workers have the opportunity to become an integral part of healthcare AI-enhanced technologies, making them more aware of their new capabilities: reducing stress, improving working conditions, and improving patient outcomes, barriers to widespread AI adoption will gradually disappear.
The above is the detailed content of Barriers to widespread adoption of artificial intelligence in healthcare. For more information, please follow other related articles on the PHP Chinese website!

Hot AI Tools

Undresser.AI Undress
AI-powered app for creating realistic nude photos

AI Clothes Remover
Online AI tool for removing clothes from photos.

Undress AI Tool
Undress images for free

Clothoff.io
AI clothes remover

Video Face Swap
Swap faces in any video effortlessly with our completely free AI face swap tool!

Hot Article

Hot Tools

Notepad++7.3.1
Easy-to-use and free code editor

SublimeText3 Chinese version
Chinese version, very easy to use

Zend Studio 13.0.1
Powerful PHP integrated development environment

Dreamweaver CS6
Visual web development tools

SublimeText3 Mac version
God-level code editing software (SublimeText3)

Hot Topics
 1386
1386
 52
52
 Bytedance Cutting launches SVIP super membership: 499 yuan for continuous annual subscription, providing a variety of AI functions
Jun 28, 2024 am 03:51 AM
Bytedance Cutting launches SVIP super membership: 499 yuan for continuous annual subscription, providing a variety of AI functions
Jun 28, 2024 am 03:51 AM
This site reported on June 27 that Jianying is a video editing software developed by FaceMeng Technology, a subsidiary of ByteDance. It relies on the Douyin platform and basically produces short video content for users of the platform. It is compatible with iOS, Android, and Windows. , MacOS and other operating systems. Jianying officially announced the upgrade of its membership system and launched a new SVIP, which includes a variety of AI black technologies, such as intelligent translation, intelligent highlighting, intelligent packaging, digital human synthesis, etc. In terms of price, the monthly fee for clipping SVIP is 79 yuan, the annual fee is 599 yuan (note on this site: equivalent to 49.9 yuan per month), the continuous monthly subscription is 59 yuan per month, and the continuous annual subscription is 499 yuan per year (equivalent to 41.6 yuan per month) . In addition, the cut official also stated that in order to improve the user experience, those who have subscribed to the original VIP
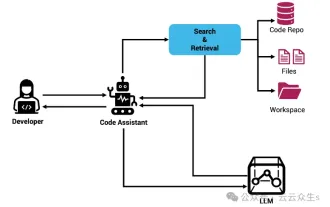 Context-augmented AI coding assistant using Rag and Sem-Rag
Jun 10, 2024 am 11:08 AM
Context-augmented AI coding assistant using Rag and Sem-Rag
Jun 10, 2024 am 11:08 AM
Improve developer productivity, efficiency, and accuracy by incorporating retrieval-enhanced generation and semantic memory into AI coding assistants. Translated from EnhancingAICodingAssistantswithContextUsingRAGandSEM-RAG, author JanakiramMSV. While basic AI programming assistants are naturally helpful, they often fail to provide the most relevant and correct code suggestions because they rely on a general understanding of the software language and the most common patterns of writing software. The code generated by these coding assistants is suitable for solving the problems they are responsible for solving, but often does not conform to the coding standards, conventions and styles of the individual teams. This often results in suggestions that need to be modified or refined in order for the code to be accepted into the application
 Can fine-tuning really allow LLM to learn new things: introducing new knowledge may make the model produce more hallucinations
Jun 11, 2024 pm 03:57 PM
Can fine-tuning really allow LLM to learn new things: introducing new knowledge may make the model produce more hallucinations
Jun 11, 2024 pm 03:57 PM
Large Language Models (LLMs) are trained on huge text databases, where they acquire large amounts of real-world knowledge. This knowledge is embedded into their parameters and can then be used when needed. The knowledge of these models is "reified" at the end of training. At the end of pre-training, the model actually stops learning. Align or fine-tune the model to learn how to leverage this knowledge and respond more naturally to user questions. But sometimes model knowledge is not enough, and although the model can access external content through RAG, it is considered beneficial to adapt the model to new domains through fine-tuning. This fine-tuning is performed using input from human annotators or other LLM creations, where the model encounters additional real-world knowledge and integrates it
 Seven Cool GenAI & LLM Technical Interview Questions
Jun 07, 2024 am 10:06 AM
Seven Cool GenAI & LLM Technical Interview Questions
Jun 07, 2024 am 10:06 AM
To learn more about AIGC, please visit: 51CTOAI.x Community https://www.51cto.com/aigc/Translator|Jingyan Reviewer|Chonglou is different from the traditional question bank that can be seen everywhere on the Internet. These questions It requires thinking outside the box. Large Language Models (LLMs) are increasingly important in the fields of data science, generative artificial intelligence (GenAI), and artificial intelligence. These complex algorithms enhance human skills and drive efficiency and innovation in many industries, becoming the key for companies to remain competitive. LLM has a wide range of applications. It can be used in fields such as natural language processing, text generation, speech recognition and recommendation systems. By learning from large amounts of data, LLM is able to generate text
 Five schools of machine learning you don't know about
Jun 05, 2024 pm 08:51 PM
Five schools of machine learning you don't know about
Jun 05, 2024 pm 08:51 PM
Machine learning is an important branch of artificial intelligence that gives computers the ability to learn from data and improve their capabilities without being explicitly programmed. Machine learning has a wide range of applications in various fields, from image recognition and natural language processing to recommendation systems and fraud detection, and it is changing the way we live. There are many different methods and theories in the field of machine learning, among which the five most influential methods are called the "Five Schools of Machine Learning". The five major schools are the symbolic school, the connectionist school, the evolutionary school, the Bayesian school and the analogy school. 1. Symbolism, also known as symbolism, emphasizes the use of symbols for logical reasoning and expression of knowledge. This school of thought believes that learning is a process of reverse deduction, through existing
 To provide a new scientific and complex question answering benchmark and evaluation system for large models, UNSW, Argonne, University of Chicago and other institutions jointly launched the SciQAG framework
Jul 25, 2024 am 06:42 AM
To provide a new scientific and complex question answering benchmark and evaluation system for large models, UNSW, Argonne, University of Chicago and other institutions jointly launched the SciQAG framework
Jul 25, 2024 am 06:42 AM
Editor |ScienceAI Question Answering (QA) data set plays a vital role in promoting natural language processing (NLP) research. High-quality QA data sets can not only be used to fine-tune models, but also effectively evaluate the capabilities of large language models (LLM), especially the ability to understand and reason about scientific knowledge. Although there are currently many scientific QA data sets covering medicine, chemistry, biology and other fields, these data sets still have some shortcomings. First, the data form is relatively simple, most of which are multiple-choice questions. They are easy to evaluate, but limit the model's answer selection range and cannot fully test the model's ability to answer scientific questions. In contrast, open-ended Q&A
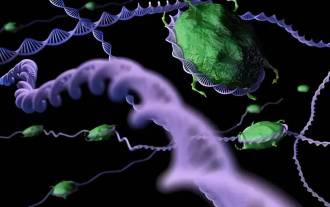 SOTA performance, Xiamen multi-modal protein-ligand affinity prediction AI method, combines molecular surface information for the first time
Jul 17, 2024 pm 06:37 PM
SOTA performance, Xiamen multi-modal protein-ligand affinity prediction AI method, combines molecular surface information for the first time
Jul 17, 2024 pm 06:37 PM
Editor | KX In the field of drug research and development, accurately and effectively predicting the binding affinity of proteins and ligands is crucial for drug screening and optimization. However, current studies do not take into account the important role of molecular surface information in protein-ligand interactions. Based on this, researchers from Xiamen University proposed a novel multi-modal feature extraction (MFE) framework, which for the first time combines information on protein surface, 3D structure and sequence, and uses a cross-attention mechanism to compare different modalities. feature alignment. Experimental results demonstrate that this method achieves state-of-the-art performance in predicting protein-ligand binding affinities. Furthermore, ablation studies demonstrate the effectiveness and necessity of protein surface information and multimodal feature alignment within this framework. Related research begins with "S
 SK Hynix will display new AI-related products on August 6: 12-layer HBM3E, 321-high NAND, etc.
Aug 01, 2024 pm 09:40 PM
SK Hynix will display new AI-related products on August 6: 12-layer HBM3E, 321-high NAND, etc.
Aug 01, 2024 pm 09:40 PM
According to news from this site on August 1, SK Hynix released a blog post today (August 1), announcing that it will attend the Global Semiconductor Memory Summit FMS2024 to be held in Santa Clara, California, USA from August 6 to 8, showcasing many new technologies. generation product. Introduction to the Future Memory and Storage Summit (FutureMemoryandStorage), formerly the Flash Memory Summit (FlashMemorySummit) mainly for NAND suppliers, in the context of increasing attention to artificial intelligence technology, this year was renamed the Future Memory and Storage Summit (FutureMemoryandStorage) to invite DRAM and storage vendors and many more players. New product SK hynix launched last year



